Accurate classification of somatic mutations is essential for meaningful interpretation and informed clinical decision-making in oncology. At Strand Life Sciences, we follow gold-standard guidelines set forth by AMP/ASCO/CAP to assess and categorize somatic variants identified through next-generation sequencing (NGS) in cancer samples, including both solid and liquid biopsies.

Variant
Detection
Evidence
Gathering
Variant
Classification
Clinical
Interpretation
AMP Tier
Categorization
Expert
Review
Strandomics aggregates and analyzes data from:


For reportable variants, our reports include clinically significant variant information including:
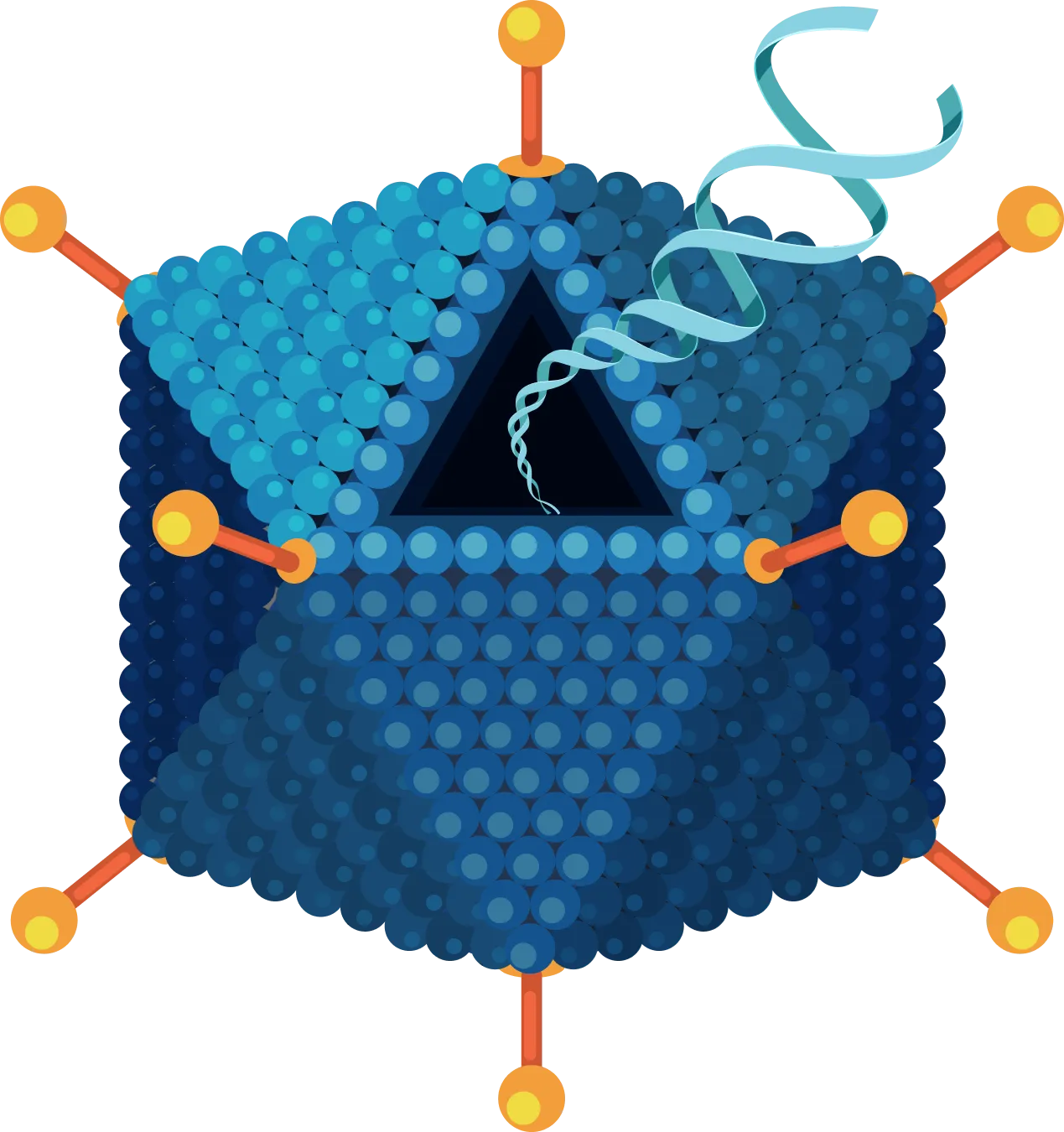
The variants are classified into four different tiers based on recommendations of the Association for Molecular Pathology (AMP), American Society of Clinical Oncology (ASCO), and College of American Pathologists (CAP) based on the strength of clinical and functional evidence.
Accurate classification of genetic variants is essential to ensure meaningful interpretation and informed clinical decision-making in hereditary cancer diagnostics. At Strand Life Sciences, we follow the gold-standard guidelines set forth by the American College of Medical Genetics and Genomics (ACMG) to assess and classify germline variants identified during testing.

Variants of Uncertain Significance (VUS) are reported with full transparency. These are variants for which current evidence is either limited, conflicting, or inconclusive regarding their role in disease.
VUSD (Variant of Uncertain Significance with probable damaging effect):
A subcategory of VUS, used when a variant shows multiple lines of evidence suggestive of a deleterious impact (e.g., predicted loss of function, deleterious in silico scores, rare in population databases), but does not yet meet the threshold for classification as Likely Pathogenic under ACMG guidelines.
Variant
Detection
Evidence
Gathering
Variant
Classification
Clinical
Interpretation
Expert
Review
Strandomics aggregates and analyzes data from:


For pathogenic and likely pathogenic variants, our reports include:




Tier I: (LOF/GOF– Strong Clinical Significance)
These variants have well-established evidence linking them to cancer development or progression. They include functionally validated mutations that are known to predict response or resistance to FDA-approved therapies and are often recommended in clinical practice guidelines.
Tier II: (LOF/GOF – Potential clinical significance)
These variants have strong functional evidence and may predict response or resistance to FDA-approved therapies used in other cancer types. They are often linked to disease and may qualify patients for relevant clinical trials.
Tier III: (Variant of Uncertain Significance)
These variants have limited, conflicting, or inconclusive evidence about their role in cancer. There is currently no strong association with disease, and their clinical impact remains unclear.
Tier IV: (Ambiguous, Likely Benign/Benign)
These variants show no evidence of contributing to cancer and are often found at high frequencies in the general population, suggesting they are harmless.